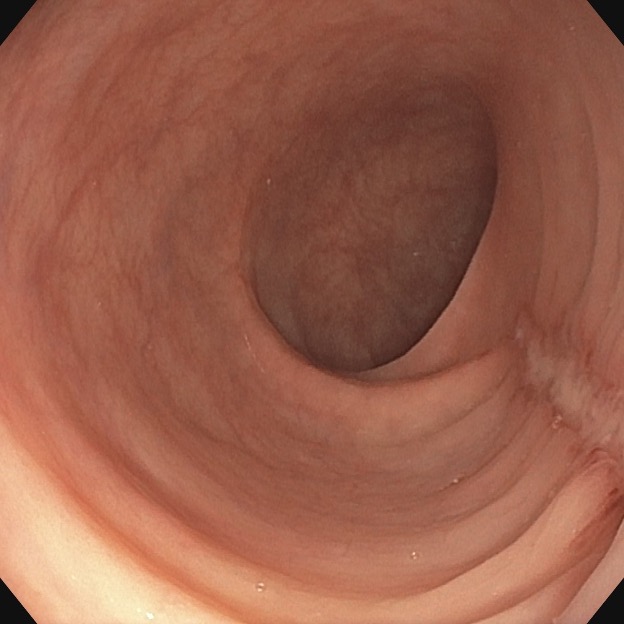
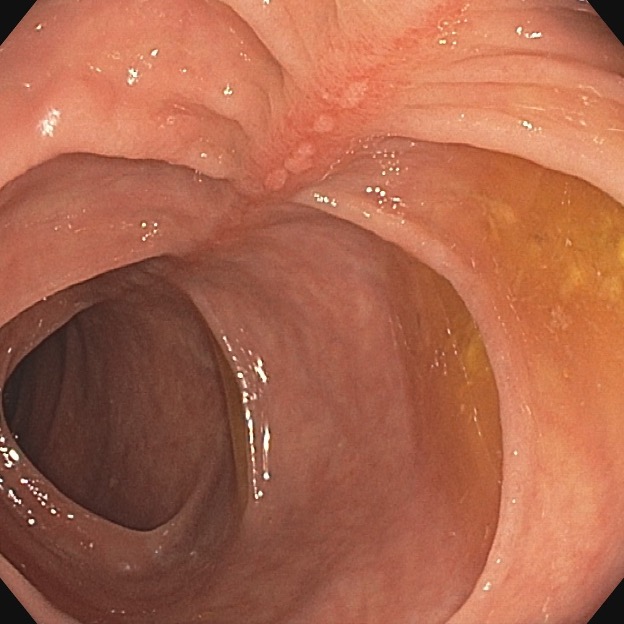
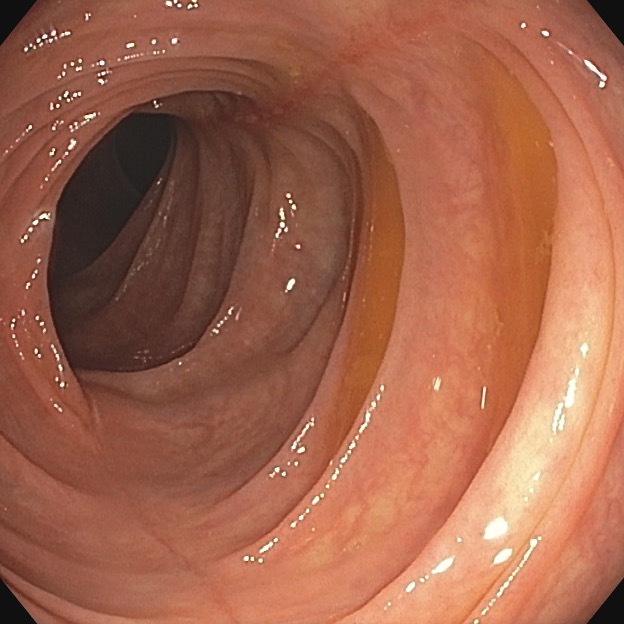
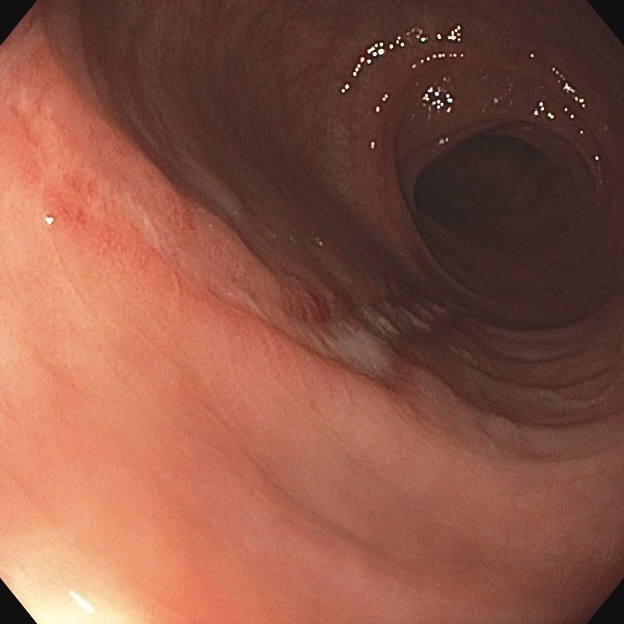
Case 22.1 Linear Colonic Ulcers
Submitted By Colin Feuille, MD
A 62-year-old woman with history of coronary artery disease status post stents, hypertension, overweight, dyslipidemia, and osteoarthritis presents with constipation, lower abdominal pain, and bloody stools. She uses polyethylene glycol most days and does not have a daily bowel movement. She has lower abdominal pain before a bowel movement which is relieved by bowel movements. For the last month or so, she has noticed bright red blood mixed in the stool occasionally. She tries to eat a high fiber diet and drink plenty of water. In the last few months, she has also noticed worsening postprandial abdominal pain. She has lost about 15 lbs in the last month or so, but notes that this was somewhat intentional in the setting of dietary modifications. Her current medications include aspirin for cardiovascular disease, naproxen for arthritis pain in her knees, anti-hypertensives, and a statin. She smokes a quarter pack of cigarettes per day and has been working on quitting. Her last colonoscopy was 3 years ago and showed diverticulosis, hemorrhoids, and a single diminutive hyperplastic polyp.
You perform a colonoscopy. What is your differential diagnosis of the finding in the pictures below?